
Treatment
Myasthenia gravis is a treatable neuromuscular disorder. Treatments differ for patients according to their age, overall health, severity of disease, and rate of disease progression.
Medications
Anti-cholinesterase medications
Examples include Neostigmine and Pyridostigmine. These drugs prevent breakdown of ACh and increase the accumulation of ACh at neuromuscular junctions. This improves the ability of the muscles to contract.
Numerous side effects can occur from taking these medications. These would include excessive salivation, involuntary muscle twitching (fasciculation), abdominal pain, nausea, and diarrhea. A drug called kaolin may be used with anti-cholinesterase medications to reduce gastrointestinal side effects.
Corticosteroids
An example of a corticosteroid is Prednisone. This suppresses antibodies that block the acetylcholine receptor (AChR) at the neuromuscular junction and may be used in conjunction with anti-cholinesterase. Corticosteroids improve symptoms within a few weeks and once improvement stabilies, the dose is slowly decreased.

A low dosage of corticosteroids might be administered indefinitely to treat MG; however side effects such as gastric ulcers, osteoporosis (bone thinning), weight gain, high blood sugar (hyperglycemia) and increased risk for infection may develop over the long term.
Image Courtesy of
https://www.flickr.com/photos/bartificial/122164551/
under a creative commons license
Immunosuppressants
Examples of immunosuppressants include Azathioprine and Cyclophosphamide. They are used to treat generalised MG when other medications fail to reduce symptoms. Severe side effects may include low white blood cell count (leukopenia), liver dysfunction, nausea, vomiting, and hair loss.
Immunosuppressants are not used to treat congenital MG because this condition is not the result of an immune system malfunction.
Other Treatments
Plasmapheresis
This is plasma exchange and is used to modify the immune system malfunction. It can be used to treat severe worsening of symptoms (exacerbations) or in preparation for surgery (thymectomy).
Plasmapheresis involves blood removal from the body and blood cells are separated from the liquid portion of the blood (plasma). Then, AChR antibodies are removed and blood cells are diluted with artificial plasma - usually a solution of saline and sterilized human albumin protein and infused back into the body.
Typically, 2 to 3 liters of plasma is removed and replaced during a single treatment. This takes up to several hours. Most patients undergo several sessions over the course of 2 weeks or more. Plasmapheresis improves MG symptoms within days and improvement lasts 6–8 weeks.
Risks include low blood pressure, dizziness, blurred vision, and formation of blood clots (thrombosis).
Thymectomy
This is su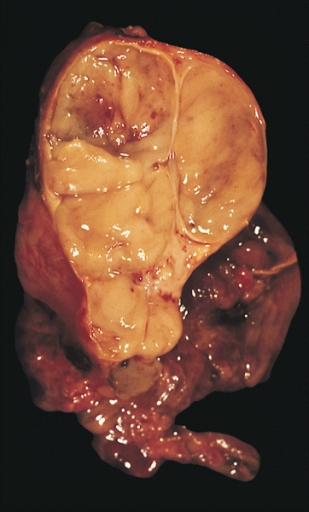 rgical removal of the thymus gland.
rgical removal of the thymus gland.
It is usually performed on patients with a tumor of the thymus (thymoma) and patients younger than age 55 with generalized MG.
Benefits of thymectomy develop gradually and most improvement occurs years after the procedure is performed.
Image Courtesy of
https://commons.wikimedia.org/wiki/File:Encapsulated_thymoma.jpg
This image is in the public domain and thus free of any copyright restrictions.
Contact
Search site
Did you know...
MG is considered a sporadic disease, meaning that it seems to strike at random and it does not run in families. There is no racial predominance, but in those who have it below 40 years old, 75% are women.